The whole mainstream narrative around C-sections based on poorly controlled observational studies reminds me strongly of the debate over whether IVF is bad for children.
We know the IVF patient population has unusually high rates of health issues and that those issues are heritable, yet most analyses do not properly control for those differences when assessing whether IVF itself causes harm.
There's basically three plausible ways in which IVF could theoretically impact the health of future children:
As far as de-novo point mutations go, well-designed studies such as Smits et al. show no statistically significant difference in point mutation rates.
Aneuploidy can be screened quite well by PGT-A, which is already a routine part of over 50% of IVF cycles.
So that just leaves the last one, where it's pretty difficult to separate the effects of IVF itself from exogenous factors like the health and infertility status of those who choose to go through it. My sense from reading the literature is that the effects, if they exist, are very small.
Yet I still see many articles like this one claiming that IVF itself causes worse health outcomes, essentially relying on nothing more than the observed correlation between IVF use and health issues.
It's maddening how statistically illiterate many mainstream scientists at well-known institutions are. If you google "does IVF cause worse health outcomes" you'll find three articles about cancer risk or "late life health problems". What is the proposed mechanism here? Cancer is caused by very specific mutation pathways that lead to uncontrolled cell growth. IVF babies have no increased risk of point mutations, and aneuploidy doesn't cause cancer.
This is all to say that I really appreciate posts like this one that actually tries to control for exogenous factors. It's surprisingly rare to see people take this approach.
This article claims "different embryo culture media give rise to different birthweights and growth patterns in children" and "children born after ART have altered epigenetic profiles".
I'm not an expert but I read it and found it quite plausible that there are ways that IVF can cause worse health outcomes. Would love to read a thorough critique of it!
Interesting study, thanks for the link.
Most of the differences listed in this analysis are basically retrospective cohort studies comparing outcomes of parents who sought IVF with those of parents who didn't. I think these are likely to result in spurious hypothesis about negative effects of IVF. We know that parents who seek IVF are disproportionately unhealthy, and as such are likely to pass on their conditions to their children.
But I'd make on exception to this generality, which is the differences observed when using different culture media. In particular, the study from Kleijkers et al, which was a double-blind RCT of 836 couples. You almost never get a randomized study that large in IVF.
It found a difference in birth weight of 158 grams between children born using two different culture media. That's a difference of about 4-6%.
That's a relatively small effect. For comparison, women with preeclampsia who give birth early tend to have babies with birth weights about 350g below that of babies born to mothers without the condition (when matching for gestational age).
So while the effect is not very large, I believe it.
What is the proposed mechanism here? Cancer is caused by very specific mutation pathways that lead to uncontrolled cell growth.
If I wanted to hypothesize a possible mechanism, an increased number of transposons might be a possible mechanism. There's "transcriptional reactivation of retrotransposons in the early mammalian embryo" and it's plausible that the deactivation happens later in a cultured embryo.
Super useful, I would love to read more of your IVF thoughts if they're posted somewhere! I think your views imply that these new sperm obstacle courses, based on fears of a worse sperm-selection process in IVF, have zero effect on people's eventual outcomes (conditional on viability)? But curious what you think. Example: "The SPARTAN system uses a series of obstacles on a microchip, requiring sperm to swim around pillar-shaped objects and through the device. As a result, this device promotes the collection of the highest quality sperm."
I'm writing a post on how to have polygenically screened children. I'll ping you when it goes up.
Well it has been 7 long months since I wrote this comment and you may have lost interest, but the post is finally up
Tangential to the content but not the title: could an acceptance of C-sections encourage women to have children in the first place? How much does the pain of natural childbirth affect willingness to have any children at all? Depending on how much you value nativity this could significantly overshadow the first-order effects.
Great question, I really want to know the answer! This study says "13% of non-gravid [not pregnant] women report fear of childbirth sufficient to postpone or avoid pregnancy." Separately, roughly 15% of women never have children, so that puts a ceiling on how big the effects could be on having any children. I suspect fear of childbirth is not a top reason for the 15%...but that's not based on much data.
A woman with one kid might choose not to have a second kid because of the unpleasantness of childbirth, after directly experiencing it, which might be a bigger effect than just looking at women who chose to have no kids.
That said, C-sections aren't pleasant, and I'd be surprised if this was a bigger factor than the rest of pregnancy and caring for a newborn.
(Epistemic status: male, no medical education, but had some discussions about this topic)
If I understand it correctly, the greatest danger of C-section is its impact on the following pregnancies. Once you have a C-section, you almost certainly must get a C-section the next time, simply because the scar tissue makes the related body parts much less flexible, and flexibility is exactly the thing you need during childbirth. After you had two C-sections, I think the third pregnancy becomes a huge health risk either way. In other words, once you have a C-section, forget about having a big (biological) family, ever.
So, even if you contemplate C-section for your last childbirth, how confident you are that you won't change your opinion later? For example, I know couples who had two kids, felt that that was enough... but ten years later changed their minds (as the childcare became much easier) and had a third child anyway. What is the chance this might happen to you?
Before we start statistically comparing C-section vs vaginal delivery, it is worth mentioning that vaginal delivery can be done in different positions. This probably depends on country; in mine, the position almost always used in hospitals is lying on your back. If you consider human physiology, a delivery on your back means that you are pushing the baby upwards, over your tailbone. Intuitively, does that feel like a good idea? The alternatives are lying on your side, pushing horizontally; or squatting, pushing downwards. (Or delivery in water, no idea what are the benefits of that.) So, if we look at the data about vaginal delivery, it makes sense to ask "which position?" because maybe the outcomes are significantly different. Similarly, there is a difference between epidural and no epidural. On one hand, it reduces the pain; on the other hand, it probably interferes with your instincts.
What I am trying to say here is that looking at a statistic that compares one value of "risk of vaginal delivery" with another value of "risk of C-section" is skipping over details that might be relevant. If you conclude that C-section is not that bad compared to the vaginal delivery, you will not explore the possibilities how to reduce the vaginal delivery risk by doing something less usual.
Anecdotally my mother is a nurse practicioner and has had me and all of my siblings via C section with zero regrets, and claims it's ridiculous that more women don't do so, so without citation I suspect the thesis here that you can't have large families is misled or confused (absent my taking a few seconds to consult the literature to actually verify).
Writing after discussion with my wife:
What I described above (vaginal delivery not recommended after C-section, pregnancy not recommended after multiple C-sections) is currently a "best practice" in my country, but there are also people who criticize this as insufficiently evidence-based. Sadly, that would not surprise me at all. :(
The keyword for this topic is "VBAC" (vaginal delivery after cesarean) for those who want to read more.
It's unclear to me why you report the 95% confidence interval for some of the results but not others.
In discussing these ideas with doctors, I get a common response that “A c-section is major abdominal surgery!”
The history of the 20th century shows a lot of cases where doctors thought they knew better and did surgeries that were not helpful for patients because of factors that were not well understood by the doctors at the time. The heuristics to avoid surgeries when possible are built on a good basis.
Major surgeries tend to often have various side effects and usually, not all side effects are measured. Scar tissue can lead to loss of flexibility in the resulting tissue which in turn leads to more stiffness and tension in the body. The loss of flexibility of a single c-section seems to be enough to be a problem for future vaginal pregnancies, I don't think it makes sense to otherwise value that flexibility at zero. Lower back pain would be one symptom that could be caused by the loss of flexibility but there are others as well.
Two arguments I heard about why c-sections might be bad for the baby are:
1) They lead to a worse gut microbiome
2) Osteopaths believe that the pressure that gets exerted during birth on the skull is part of the normal development of the skull.
Very interesting! I work in health insurance and we try to encourage vaginal delivery and discourage C-sections; the other side you present here is a surprise. Good stuff.
Summary
I think so. Correlations tend to show worse outcomes for c-sections, but the guidelines take this evidence too literally. Careful causal evidence finds that it’s more of a mixed bag. Moderate negative effects on subsequent births seem more robust. An elective c-section might be the defensible choice for someone’s final pregnancy.
Disclaimer: Not a doctor.
The official guidelines
C-sections cost about twice as much as vaginal delivery and are associated with worse health outcomes for infants and moms. These facts are concerning enough to the US Medicaid system that one of their “Improvement Initiatives” is reducing low-risk cesarean delivery. They write: “Cesarean delivery poses a greater risk of maternal morbidity and mortality for low-risk pregnancies when compared to vaginal births, a risk that ideally should be avoided.”
They lead seminars with slides like this, highlighting that everything bad is correlated with c-sections:
Hospitals have been falling in line. UCSF boasts: “Our view of labor and childbirth as a natural process has helped keep our overall Cesarean rate at 20 percent, among the lowest rates in California…Our threshold for making the decision to recommend a C-section is a lot higher than in other places.”
The American College of Obstetricians and Gynecologists (ACOG) has similar advice, and to their credit they spell out the evidence and their reasoning. The main paper they cite is this Canadian study of 2.3m vaginal and 46k c-section deliveries. “A large population-based study from Canada found that the risk of severe maternal morbidities…was increased threefold for cesarean delivery as compared with vaginal delivery.”
But what really should we make of the association between c-sections and bad outcomes? The observed correlation is ripe for reverse causality, for the same reason that going to the hospital is correlated with dying: c-sections are often performed because of some dangerous condition (e.g., preeclampsia). In the Canadian study, the treatment group was mothers who had scheduled a c-section due to breech position, and breech is correlated with other negative outcomes. In other studies, the c-sections could happen for reasons that are never recorded in hospital data, so even lots of control variables should make you worried about selection effects.
The causal effect of a c-section
A new paper by Card, Fenizia, and Silver, using data from California births, takes the question of causality seriously. It appears to be the only careful attempt at separating correlation and causation.
C-sections are not randomly assigned. How can we use observational data to arrive at a causal estimate? Their approach combines the facts that hospitals exhibit stable differences in their (risk-adjusted) c-section rates and that moms often give birth at the hospital closest to them.
Together, these mean that some moms will have c-sections by virtue of living close to a hospital that performs more of them. In essence, a causal estimate can be derived by comparing the outcomes of mothers who live near vs. far from high c-section hospitals.
You might be concerned that certain kinds of moms live next to certain kinds of hospitals. But in detailed tests, the authors find no signs of problematic selection along this distance-to-hospital dimension (although with these kinds of designs it’s reasonable to worry that something not measured could still bias the estimates).
And they show that the distance measure does have a large effect on c-sections for the group they study: low-risk first births. (Why restrict to this sample? High-risk births are often defaulted to c-sections, and a c-section in a first birth means you should probably only get c-sections in subsequent births—so this is the group that is most relevant to the policy discussion.)
With this distance-based variation in hand, the authors estimate causal effects on a range of infant and maternal outcomes. Contrary to the correlational evidence, the estimates are mixed.
C-section babies have:
Mothers who get c-sections have:
Importantly, these results only apply to marginal cases: mothers whose delivery method was determined by the practices at the hospital. But this is arguably the perfect subgroup to study for the current debate about c-section rates. Remember the “threshold” that the UCSF doctor mentioned. Should it be higher or lower?
Also, these outcomes are limited; there’s lots more that we’d want to know. The study is under-powered to look at other consequences for the mothers (including mortality, although see notes at bottom) and does not have the data to look at long-run consequences for either mothers or children.
But this should all be very surprising and possibly concerning to the people putting those presentations together for Medicaid. Instead of c-sections being clearly bad for low-risk births, the conclusion here is that it is far from obvious—you trade some problems for other problems.
The favorable result in the Apgar score, which measures how lively the baby is just after birth, seems consistent with the mechanics of the two delivery methods. With vaginal birth, the baby can get stuck. This kind of problem is less likely with c-sections. This is also an imminently critical outcome: some babies with low Apgar scores will have permanent brain damage from hypoxic ischemic encephalopathy.
The respiratory issues for c-section babies also line up with a recent assessment which singles out “delayed clearance of lung liquid” as a culprit, although it seems more mysterious.
The outcomes for mothers are a little hard to piece together. The outcome I put most weight in is length of stay, as this should capture most of the very bad things depicted in the Medicaid slide above. The insignificant but positive estimates on emergency room visits, even taken at face value, are much smaller than the estimates in the Medicaid slide, which all suggest a doubling of risk or more.
Finally, for what it’s worth, the flat results for mothers and infants line up with a randomized trial of twin pregnancies: “planned cesarean delivery did not significantly decrease or increase the risk of fetal or neonatal death or serious neonatal morbidity, as compared with planned vaginal delivery," and "We did not find that planned cesarean delivery was associated with a higher or lower risk of maternal death or serious maternal morbidity than planned vaginal delivery."
Subsequent pregnancies
The ACOG guidelines are actually more worried about effects on subsequent pregnancies: “the downstream effects are even greater because of the risks from repeat cesareans in future pregnancies.” The main theory, from what I can tell, is that the c-section scar interferes with the formation of the placenta, resulting in placental issues and preeclampsia. These are dangerous conditions that greatly increase the chance of harm for both mother and baby. There could also be subtler issues getting nutrients to the baby that don’t register in checks of maternal health.
Their reference for this is Silver et al. I’m a little stunned at how simplistic the analysis is. They only study c-section births and look at the correlation between negative outcomes and the number of previous births. The problem is that all of this could just be a birth order effect, not a number-of-previous-c-sections effect. Second, while they find increased risk of placental malformation in subsequent pregnancies, the initial c-section might have happened because of this very issue. Surely moms who have a given issue are more likely to have it again, regardless of method of delivery.
More convincing evidence comes from Daltveit et al 2008, using Norwegian register data. They compare outcomes for the second pregnancy for women whose first birth was vaginal vs. Cesarean: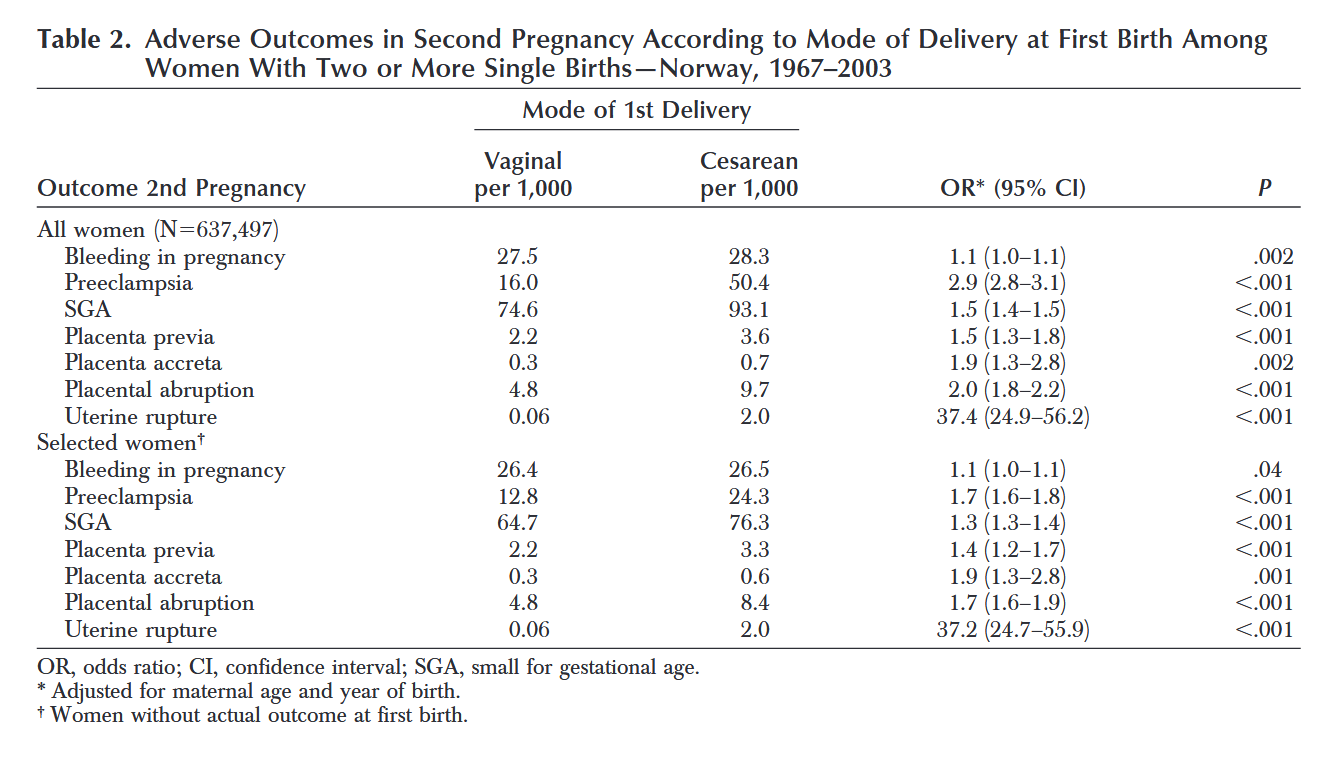
The All women comparisons don’t impose any restrictions. In the Selected women section, they leave out women who had the same condition in their first pregnancy. This addresses the important source of bias that Silver et al ignore. Still, most outcomes show a clear increase.
There are increases in preeclampsia and SGA (small for gestational age). These could be connected with malformation of the placenta. There are effects on placenta outcomes and uterine rupture, although these represent small absolute risks. The risk of placenta previa increases from 0.22% to 0.33%. The risk of uterine rupture increases from 0.006% to 0.2%.
The uterine rupture result is scary but this appears to be driven by women who attempt vaginal delivery after a c-section—something the authors don’t account for. Another source that compares people based on their planned method finds strong evidence of this: "The estimated incidence of uterine rupture was 2 per 10,000 maternities overall; 21 and 3 per 10,000 maternities in women with a previous caesarean delivery planning vaginal or elective caesarean delivery respectively." So risks were practically the same for the caesarean-to-caesarean mothers.
One lingering confound is that, even among the Selected women, “confounding by indication” may still cause the previous c-section mothers to have worse prospects, biasing the comparison. A way around this is to look at outcomes for elective c-sections—mothers who are not getting the c-section because of a health need. This seems to show the same result. For example, in this case control study, mothers with placenta accreta were more likely to have had a previous elective c-section.
Conclusion
Where does that leave us? The Card et al paper should make us more agnostic about the costs of a c-section for a one-off, low-risk birth. But, while I could not find careful causal studies on subsequent births, the observational studies do suggest that they may suffer negative effects of a previous c-section. Based on this investigation, I now believe that choosing an elective c-section for a one-off kid, or your last pregnancy, could be the more defensible choice.
In discussing these ideas with doctors, I get a common response that “A c-section is major abdominal surgery!” From my perspective, given the tragic injuries that can befall mother and infant in the process of childbirth, Mother Nature hasn’t done herself any favors. Maybe we can, in fact, do better.
Notes
I am still looking for better cites on this, but it appears that maternal mortality for elective c-sections, is lower if anything in observational data. (Although the selection bias here could favor scheduled c-sections.)
As always, Emily Oster is the best place to start with questions like this. She believes the effects on placental malformation in subsequent pregnancies. See her thoughts here. In particular: “The good news is, if we look at one or two years after birth, there is no evidence of differences in recovery. If anything, the data might slightly favor C-sections.” In a big meta-analysis she cites, “The only two complications that differed across groups were urinary incontinence and pelvic organ prolapse. Both are actually more common for women who have had a vaginal delivery.”