Hi! I'm Aaron, Lantern Bioworks is my company.
Thanks. Similar to the concern of "could the bacteria colonize the vaginal tract after oral sex?" this is exactly the sort of edge-case risk we wanted to identify. We want to reward that safety-red-teaming by paying you $500. Send me your paypal, venmo, or crypto address at your leisure.
(The bug bounty is still $100 by default, but this was high-effort and we appreciate it. If anyone has more potential bugs to submit, email me at aaron@lanternbioworks.com !)
Re: elevated oral cancer risk in ALDH-deficient populations—I asked our dentech advisor Dr. Justin Merritt about it, and he said approximately,
The acetaldehyde cancer risk they describe is legit for AFR populations. However, connecting that risk to Lumina-derived ethanol production is where the argument becomes suspect.
Their argument is that a cariogenic diet (ie, sugar-rich) might produce sufficient ethanol in the mouth from Lumina to trigger local acetaldehyde production that damages the local epithelium; that the admittedly small total amounts of ethanol produced by Lumina might yield high local concentrations of acetaldehyde in the adjacent epithelium.
Firstly, S. mutans does not colonize the epithelium. It lives almost exclusively on enamel. The total surface area in the mouth that it could realistically inhabit is exceptionally small, unless Lumina can live in places that S. mutans generally does not. Other oral strep species overwhelmingly occupy the majority of epithelial surfaces of the mouth, which effectively restricts S. mutans to the teeth. This means that any miniscule quantities of ethanol produced by Lumina on enamel would be diluted by saliva before ever reaching the epithelium. Likewise, if other coinhabiting microbiota convert Lumina ethanol to acetaldehyde, this too would be diluted by saliva before reaching the epithelium.
Or, if one argues that Lumina could float around in saliva and affect oral epithelium by producing ethanol, I think this would be a dubious argument as well. Firstly, bacteria in saliva are transient, as they get swallowed. Secondly, the numbers just don't add up in my mind. The saliva of people with extreme caries risk have 10^6 CFU/ml S. mutans detectable in saliva. At that concentration of bacteria (which is already quite rare), one could not even visibly detect turbidity in liquid. That shows how few S. mutans are present relative [to] the large volume of the mouth (i.e., it's a pretty small quantity of ethanol production potential and even this level would only persist when sugar levels are high in saliva). S. mutans generally can only achieve high concentrations of bacteria in those specific places you tend to see caries develop, like the pit and fissures of the molars or interproximally.
The article makes a logical argument, but I suspect the actual risk is nowhere even close to what they propose. There are a number of estimates and guesses included in the article that may not pan out in reality. Fundamentally, the risks associated with Lumina-derived ethanol is miniscule compared to normal ethanol consumption. Is it possible that one who abstains from alcohol consumption could still be at risk due to Lumina ethanol production? I suppose it is possible, but I find it extremely unlikely.
Firstly, S. mutans does not colonize the epithelium. It lives almost exclusively on enamel. The total surface area in the mouth that it could realistically inhabit is exceptionally small, unless Lumina can live in places that S. mutans generally does not.
Big crux! Thanks for the investigative effort. Sounds mostly resolvable via assay of existing Lumina customer saliva.
An interesting twist: drinking ethanol doesn't just cause acute exposure but "The concentration of ethanol in the oral cavity increases immediately after an alcoholic beverage is consumed and then decreases. It was reported after intake of an alcoholic beverage that the concentration of ethanol remaining in the oral cavity decreases gradually, as ethanol flows back into saliva from the blood for a few hours after it is taken into the body [25,26]. Most previous studies of acetaldehyde production by oral bacteria, including our study [24], used ethanol concentrations as low as 11–22 mM (approximately 0.05–0.1%), which corresponds to the ethanol concentrations seen in saliva a few hours after alcohol consumption [20,22,26,27]. " From https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8204988/
What you are missing here is that S. mutants often lives in pockets between tooth an epithelium or between teeth with direct permanent contact to epithelium. Due to the geometry of these spaces access to saliva is very poor so metabolites can enrich to levels way beyond those you suggest here.
This mechanism is also a big problem with the pH study above.
I can confirm that my PayPal has received the $500, although it'll be frozen for a while.
Thanks! I had a lot of fun doing the research for this and I'm working on an update that'll be out in a few days.
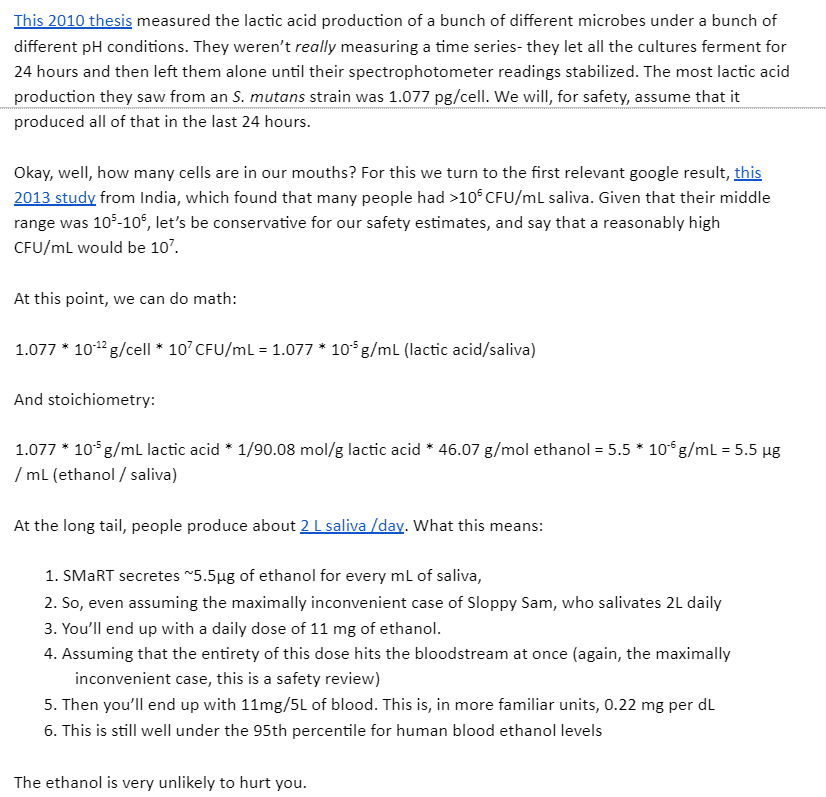
My understanding is that the amount of ethanol we're taking about here on a daily basis constitutes something like the amount you'd get eating an extra piece of fruit or so. Though I don't know where I originally saw the estimate or if it is good. Does anyone want to do some fermi estimates?
This is from the Google Doc FAQ.
It's bad for a bunch of reasons. Firstly, the rate of metabolism decreases as pH decreases - and the main product was lactic acid, which decreases pH. Second, they only considered bacteria in saliva. There are far more bacteria attached to your epithelium and teeth than there are in your saliva, since you swallow your saliva several times a minute.
Finally, there's the fact that the entire reason this project exists is to change the product of sugar fermentation from lactic acid to ethanol in order to prevent tooth decay. Lactic acid can only cause tooth decay if local pH is below 5.5. A similar amount of ethanol would be ~2% by mass. I'm pretty sure AFR people who only drink beer still have an elevated oral cancer risk. And that's with only a few minutes of exposure a day! Consider what would happen if someone had that level of exposure every time they ate any carbs.
Thanks, this is interesting.
My understanding is that cavities are formed because the very local pH on that particular sub-part of the tooth is below 5.5. IIUC teeth can't get cancer. Are you imagining Lumina colonies on the gums having this effect there, the Lumina colonies on the teeth affecting the general oral environment (which I think would require more calculation than just comparing to the hyper-local cavity environment) or am I misunderstanding something?
I was thinking of areas along the gum-tooth interface having a local environment that normally promote tooth demineralization and cavities. After Lumina, that area could have high chronic acetaldehyde levels. In addition, the adaption of oral flora to the chronic presence of alcohol could increase first-pass metabolism, which increases acetaldehyde levels locally and globally during/after drinking.
I don't know how much Lumina changes the general oral environment, but I think you might be able to test this by seeing how much sugar you can put in your mouth before someone else can smell the fruity scent of acetaldehyde on your breath? I'm sure someone else can come up with a better experiment.
Thanks! This is much closer to the amount of ethanol you'd get eating 50 bananas a day. That's at least one sanity check it fails then, even under these ideal conditions since, as you noted, there is probably a larger bacteria population than what was measured there.
Now I'm wondering about sanity checks in the other direction though. Is ~.5 ml per hour of ethanol actually a realistic production?
If it's really more like 10^6 and not 10^7 that's five bananas worth and not something I would worry about. Isn't this resolvable via saliva assay?
I'm not convinced. The amounts of alcohol involved are very small and people with this deficiency are not told to stay away from alcohol no matter what.
I don't think the comparison with lactic acid is adequate - alcohol is a much more common substance, which is present in small concentration basically everywhere. I just think that the quantity is very small to matter, even with the "local" argument.
So what? It still comes from ethanol. Again, people with this deficiency are not told to stay away from alcohol no matter what.
Even when the acetaldehyde itself increase oral cancer, parodontitis also increases oral cancer rates. While Lumina won't completely removes parodontitis, reduced pardontitis might reduce oral cancer rates in the same amount as the increased acetaldehyde increases it resulting in net zero effect.
As a useless anecdote, I took Lumina in November of last year. I generally drink a lot, and have commented on hangovers getting 2-4x worse in the past few months to friends, before reading this post or knowing anything about your hypothesis. This has occurred only in the last few months and I'm 24 years old.
It would be ironic if that turned out to be true, but because of our apparent Western cultural cycle right now being anti-alcohol, came to be regarded as a feature of the Lumina bacteria rather than a bug (of the bugs).
Interesting. I took Lumina around December and have noticed no change, though I don't think I've actually been hungover during that time period. I definitely didn't notice any difference in the AMOUNT needed to produce a hangover; I drunk a substantial amount and didn't get hangovers any more easily.
It might have conditioned your oral and gut flora to break down ethanol into acetaldehyde faster. I'll have a follow-up piece on hangovers and AFR coming soon, but the short of it is that certain antacids taken before drinking may help by decreasing ethanol first pass metabolism.
I looked a little into the literature on how much alcohol consumption actually affects rates of oral cancers in populations with ALDH polymorphism, and this particular study seems to be helpful in modelling how the likelihood of oral cancer increases with alcohol consumption for this group of people (found in this meta-analysis).
The specific categories of drinking frequency don't seem to be too nice here, given that it was split between drinking <=4 days a week, drinking >=5 days a week and having less than 46g of ethanol per week, and drinking >=5 days a week and having more than 46g of ethanol per week. Only in the latter category was there an actual significant increase in oral cancer rates (4.4x), although there is some non-significant evidence for about a 1.5x increase in the high-moderate group and the moderate group. Comparing the ~77 mg/week ingestion rate from the document to the 10-40g range I would estimate the high-moderate group to have, I would imagine that there is probably a much more minor effect for Lumina (if I had to estimate, maybe like a 1.1x risk, which might be offset by the benefits of lower levels of lactic acid at that level).
One other argument against this (which I would put a lower epistemic status on given my basic intuition of enzyme kinetics) would be that since people probably tend to have more than 10 milligrams of alcohol every time they have a gulp of an alcoholic beverage, ALDH2 deficiency would be much more of a bottleneck as acetaldehyde levels rise rapidly after consuming alcohol compared to the rather low background generation of acetaldehyde we might see for Lumina users.
As I am being slightly a "man of one study" here, I'd be interested to see if you've found any studies of your own that demonstrate more of an effect of alcohol consumption on oral cancer for ALDH2 deficiency than I've been listing here.
There are a lot of studies to regarding the assocation between ALDH2 deficiency and oral cancer risk. I think part of the issue is that
- AFR people are less likely to become alcoholics, or to drink alcohol at all.
- Japanese in particular have a high proportion of ALDH2 polymorphism, leading to subclinical but still biologically significant levels of acetaldehyde increase after drinking among the non-AFR group.
- Drinking even small amounts of alcohol when you have AFR is really really bad for cancer risk.
- Note that ALDH2 deficiency homozygotes would have the highest levels of post-drinking acetaldehyde but have the lowest levels of oral cancer because almost none of them drink. As in, out of ~100 homozygotes, only 2 were recorded as light drinkers, and none as heavy drinkers. This may be survival bias as the definition of heavy drinking may literally kill them.
- The source for #4 looks like a pretty good meta-study, but some of the tables are off by one for some reason. Might just be on my end.
- ADH polymorphism is also pretty common in Asian populations, generally in the direction of increased activity. This results in faster conversion of ethanol to acetaldehyde, but often isn't included in these studies. This isn't really relevant for this discussion though.
As always, biostatistics is hard! If X causes less drinking, drinking contributes to cancer, and X increases drinking's effects on cancer, X may have positive, neutral, or negative overall correlation with cancer. Most studies I've looked at had a pretty string correlation between ALDH2 deficiency and cancer though, especially after you control for alcohol consumption.
It also looks like most researchers in the field think the relationship is causal, with plausible mechanisms.
The oral flora contains a diversity of organisms, bacterial, viral, and fungal, including some yeasts. Don't some of them produce ethanol already? And adhere to the mucous membrane instead of enamel? It wouldn't surprise me if some even excrete acetaldehyde under some conditions. Is Lumina really such a change?
UPDATE: Two boxed vials of the Lumina treatment arrived in the mail for me last week. I've put them in the fridge for best shelf life and plan to bring one to my next cleaning. I got my wisdom tooth surgery over a decade ago, and to the best of my knowledge I have no active caries.
I am an Asian ~30yo man (ethnically Korean, specifically) who has suffered from bad cavities all his life and who also suffers from Asian glow to the point of it being uncomfortable to drink; I am also planning to get the Lumina treatment. I do not think that the amount of alcohol produced is particularly relevant; I drink occasionally and eat a ton of fruit, and thus I think that my marginal risk is basically negligible.
I don't smoke, and to the best of my knowledge, I have no particular family history of cancer, let alone oral/esophageal cancer, despite high rates of smoking in my family history.
As such, I'm pretty sure that the expected value calculation is overdetermined towards "get the Lumina", given how unpleasant caries and carie treatment are for me and the (weak but maybe real?) connection between caries and Alzheimer's. Given a choice of damnations, I think I'd prefer oral cancer to Alzheimer's even with ~identical proportional changes in likelihood; given how dubious I am on the marginal risk of oral cancers to start with, I'm only that much more set on fixing my oral microbiome.
If anyone wants me to take measurements or keep data or logs of observations, please let me know.
I certainly agree that I'd hold off until I knew the answers to a bunch more questions.
This all seems to rest on the relative increase in oral and esophygeal cancer. 10x sounds like an awful lot. But in terms of decision-making, the absolute increase, not the ratio, is the bottom line. So: what are the absolute likelihoods? If they're both miniscule, this might not be a deciding factor. Increasing my cancer risk by one in a million might be a good trade for immunity to cavities and gum disease.
If you throw in immunity to bad breath, I'd take that deal. I wonder how large a factor the alcohol vs lactic acid is in bad breath.
I think it's also worth considering how much ethanol is excreted into the mouth by these bacteria relative to how much in the mouth of a heavy drinker. I'm sure the frequency vs. persistance is also a factor, but I'm not sure how.
On the other hand, if those numbers are much higher, it's possible that even those without ALDH deficiency shouldn't take the treatment.
a good trade for immunity to cavities and gum disease.
If you throw in immunity to bad breath
FYI, https://www.luminaprobiotic.com/faq says used to say
This strain doesn't do anything to protect against gum disease, or bad breath.
Does it? I see:
We would still recommend brushing your teeth. We don't yet know whether this strain does anything for gum disease or bad breath.
Emphasis mine.
Even if it reduces it a bit, there's no good reason to assume that it causes immunity.
Lumina is about replacing Streptococcus mutans while leaving Lactobacillus alone. Streptococcus mutans lives on dental tissue while Lactobacillus lives on the gum. Both produce lactic acid.
I'm not certain this is a big problem, but it can be. My guess is 60% that this causes a significant increase in oral cancers for ALDH deficiency heterozygotes.
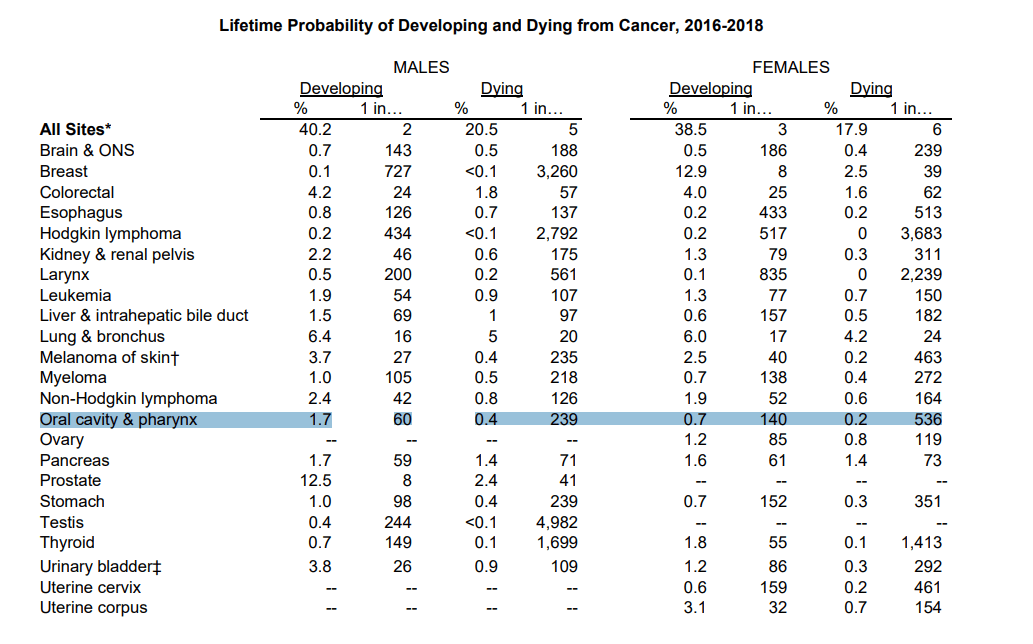
If you add up the upper digestive tract cancers, it looks like 2.7% developing and 0.8% dying for men, and 1.4% developing and 0.5% dying for women.
It's worse than cervical cancer (0.6/0.2%), even if you only consider oral/esophageal for women.
Yep, that's an alarmingly high base rate, so multiplying that by ten is an enormous added risk. So even if the concentration and effect is far lower than in alcoholics, I'd still probably not take that risk.
Possibly even without ALDH deficiency.
To make no choice is to make a choice, and to take no action is to take an action. I'd ask the flip side of Lao Mein here - how confident are you, exactly, that your current state of affairs is all that great in an absolute sense, and what are you willing to risk a small chance of in exchange for clear benefits now and in future?
Interesting.
You wrote, "Is it possible that acetaldehyde and ethanol behave differently from lactic acid? Maybe."
I'll note that they behave differently in one way: acetaldehyde has a very low boiling point, 68.36°F. That's why you can smell it so strongly on an alcoholic's breath! There's an argument that low levels of acetaldehyde produced in the mouth will evaporate into the breath quickly and constantly, while lactic acid sticks around. However, the speed at which it will evaporate is an empirical question, and I'm not confident in saying there will be no harm in people with ALDH deficiency.
There's also the question of how the biofilm will retain it, and what areas of the gums and throat will be coated in such biofilms.
If anyone is otherwise interested in the Lumina "displace harmful bacteria with less-harmful ones" approach but concerned about this alcohol metabolism issue, I have an alternative for you to investigate. Oral probiotics such as "ProBiora" have been on the market for some time, and they take the approach of introducing bacteria that compete with S. mutans while not being implicated in caries themselves. These solutions are probably less powerful than Lumina advertises itself to be, and are not permanent, which removes a bit of the "cool factor" but in my mind does not make them less valuable.
Saliva causes cancer, but only if swallowed in small amounts over a long period of time.
(George Carlin)
For this to be a risk, the cancer risk would have to be superlinear in the acetaldehyde concentration. In a linear model, the high local concentrations would not matter overall, because the expected number of mutations you get would not depend on how you distribute the carcinogen among your body cells.
Or the cells in your mouth or throat could be especially vulnerable to cancer.
From my understanding, having bacteria in your mouth which break down sugar to ethanol is not some bizarre mad science scheme, but it is something which happens naturally, as an alternative to the lactic acid pathway, and people who never get cavities naturally lucked out on their microbiome. This in turn would mean that even among teetotaler AFR patients there should be an excess of oral cancers, and ideally an inverse correlation between number of lifetime cavities and cancer rates.
On the meta level, I find myself slightly annoyed if people use image formats to transport text, especially text like the quotes from Scott's FAQ which could be easily copy-pasted into a quotation. Accessibility is probably less of an issue than it was 20 years ago thanks to ML, but this still does not optimize for robustness.
Might this be an issue even for people without this gene? What is the risk that constantly producing low levels of ethanol can cause oral cancer for ordinary people?
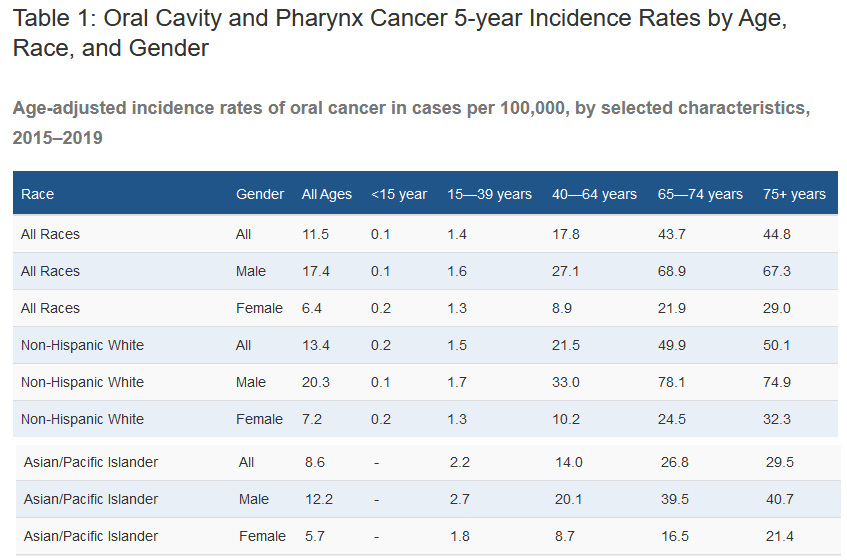
If that's the case, that seems like a huge hole in your argument/concern. But from statistics taken for the US, it looks like AAPIs get oropharynx cancers at a significantly lower rate than both non-Hispanic Whites and general population both, despite a possibly-higher rate of smoking (for cultural reasons) and a definitely-much-higher rate of defective ALDH polymorphisms.
A Japanese guy I used to work with had a very serious genetic alcohol intolerance. (Like, a single drop of wine would probably be ok but anything more than that would likely put him in the hospital).
I guess if you have a known inability to metabolise alcohol, such that you're already having be very car3fuo that anything you consume doesn't have alcohol in it, you might want to be a little bit cautious here. but ... maybe the quantity you get from the bacteria is so small it doesn't matter.
This paper seems like an interesting counterpoint: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5421578/
Estimates of Ethanol Exposure in Children from Food not Labeled as Alcohol-Containing
They find that:
... orange, apple and grape juice contain substantial amounts of ethanol (up to 0.77 g/L).
... certain packed bakery products such as burger rolls or sweet milk rolls contained more than 1.2 g ethanol [per] 100 g.
... We designed a scenario for average ethanol exposure by a 6-year-old child. ... An average daily exposure of 10.3 mg ethanol [per] kg body weight (b.w.) was estimated.
This is estimated ethanol exposure just from eating and drinking regular non-alcoholic food and beverages. A dose of 10mg/kg of ethanol is hundreds of milligrams total, per day -- more than an order of magnitude higher than the highest estimate discussed here for the bacteria.
(I will note that I had difficulty verifying any of this; there are lots of news stories on this topic, but they are all fairly fluffy, and link back to the same single study.)
The LessWrong Review runs every year to select the posts that have most stood the test of time. This post is not yet eligible for review, but will be at the end of 2025. The top fifty or so posts are featured prominently on the site throughout the year.
Hopefully, the review is better than karma at judging enduring value. If we have accurate prediction markets on the review results, maybe we can have better incentives on LessWrong today. Will this post make the top fifty?
Update: further research has led me to believe that people of all races should test themselves for ALDH deficiency before using Lumina. Even if you don't exhibit AFR symptoms when drinking alcohol, your ALDH activity may still be decreased.
Many people in the rational sphere have been promoting Lumina/BCS3-L1, a genetically engineered bacterium, as an anti-cavity treatment. However, none have brought up a major negative interaction that may occur with a common genetic mutation.
In short, the treatment works by replacing lactic acid generating bacteria in the mouth with ones that instead convert sugars to ethanol, among other changes. Scott Alexander made a pretty good FAQ about this. Lactic acid results in cavities and teeth demineralization, while ethanol does not. I think this is a really cool idea, and would definitely try it if I didn't think it would significantly increase my chances of getting oral cancer.
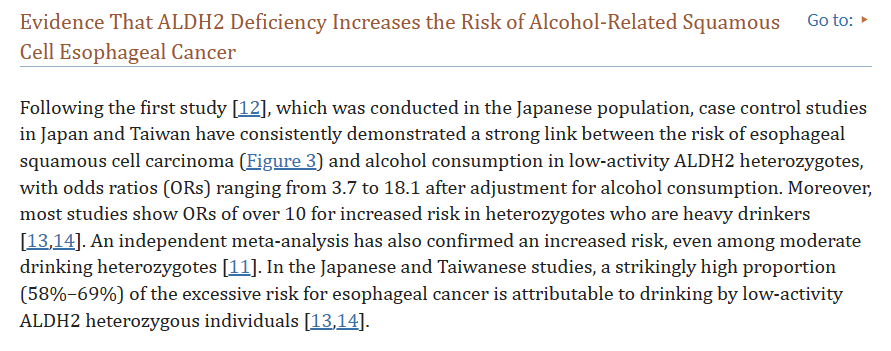
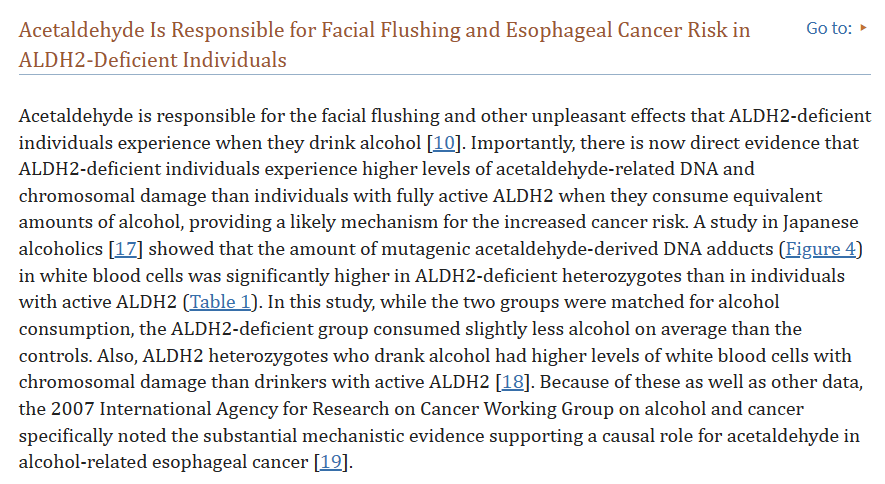
Why would that be? Well, I, like around half of East Asians, have a mutation in my acetaldehyde dehydrogenase (ALDH) which results in it being considerably less active. This is known as Asian/Alcohol Flush Reaction (AFR). This results in decreased ability to metabolize acetaldehyde to acetate and consequently a much higher level of acetaldehyde when drinking alcohol. Although the time ingested ethanol spends in the mouth and stomach are quite short, alcohol dehydrogenase activity by both human and bacterial cells rises rapidly once the presence of ethanol is detected. Some studies have estimated that ~20% of consumed ethanol is converted to acetaldehyde in the mouth and stomach in a process called first pass metabolism. Normally, this is broken down into acetate by the ALDH also present, but it instead builds up in those with AFR. Acetaldehyde is a serious carcinogen and people with AFR have significantly higher levels of oral and stomach cancer (The odds ratios for Japanese alcoholics with the mutation in relation to various cancers are >10 (!!!) for oral and esophageal cancer). The Japanese paper also notes that all alcoholics tested only had a single copy of the mutation, since it is very difficult to become an alcoholic with two copies (imagine being on high dosage Antabuse your entire life - that's the same physiological effect).
In addition, there is also the potential for change in oral flora and their resting ADH levels. As oral flora and epithelial cells adapt to a higher resting level of ethanol, they may make the convertion of ethanol to acetaldehyde even faster, resulting in higher peak oral and stomach levels of acetaldehyde during recreational drinking, thereby increasing cancer risk.
There is also the concern of problems further down the digestive track - Japanese alcoholics with AFR also have increased (~3x) colorectal cancer rates, which may well be due to ethanol being fermented from sugars in the large intestines, but my research in that direction is limited and this article is getting too long.
While others have argued that the resulting acetaldehyde levels would be too low to be a full body carcinogen (they make a similar calculation in regards to ethanol in this FAQ), my concern isn't systemic - it's local. AFR increases oral and throat cancer risks most of all, and the first pass metabolism studies imply that oral and gastral acetaldehyde are elevated far above levels found in the blood.
As a thought experiment, consider that a few drops of concentrated sulfuric acid can damage your tongue even though an intraperitoneal (abdominal cavity) injection of the same would be harmless - high local concentrations matter! The same is true for concentration in time - the average pH of your tongue on that day would be quite normal, but a few seconds of contact with high concentrations of acid is enough to do damage. This is why I'm not convinced by calculations that show only a small overall increase in acetaldehyde levels in the average person. A few minutes of high oral acetaldehyde levels a day is enough to cause oral cancer - that's how it works in people with AFR when they drink alcohol!
But perhaps the increase in acetaldehyde is simply too low to cause significant problems, even in the mouth? I think this is possible, but unlikely. The reason Lumina was created at was because of cavities. Most oral bacteria convert sugars to lactic acid as the end product of anaerobic metabolism. This results in cavities when mouth pH is lowered below 5.5. My back-of-envelope calculation say that this implies a 0.01 mol solution of lactic acid, or about 5% by mass. This may well be even higher in practice since saliva acts as a pH buffer. Note that while resting saliva samples rarely measure below 6.3 pH, it can drop down to 4.0 after drinking certain sugary drinks (somehow, this topic is underresearched. Is this why people complain about dental science?). Notably, this is caused by sugar metabolism. Sour milk, sugarless coffee, and light (diet) coke resulted in much higher oral pHs than their sugary counterparts. Again, transient local exposure of oral epithelium to acetaldehyde is exactly what causes the elevated oral cancer risk in the first place, and similar exposure to lactic acid is what causes cavities. Is it possible that acetaldehyde and ethanol behave differently from lactic acid? Maybe. But the weight of evidence is enough to make me concerned.
All considered, I personally consider the negatives of potential cancer risk greater than the positives of cavity prevention for someone with AFR. I would recommend further research on oral acetaldehyde for people with and without ALDH deficiency who have already taken the treatment, advice against the use of Lumina for those known to have the mutation, and urge those of East Asian ancestry to test themselves if they are unsure. As a reminder, ALDH deficiency is a semi-dominant mutation - you may have the phenotype even if you have a low East Asian admixture.
Excerpts from Scott's FAQ follow:
Conflict of Interest: If you've already used Lumina and regularly kiss Asians, this may be a concern. However, my interest in kissing women outweighs my interest in not having cancer, so I recommend no change in behavior.
My recommendations would be:
Update: I am reminded that ALDH polymorphism isn't restricted to Asians, and that many variants which don't heavily disrupt drinking can still result in significant increases in acetaldehyde levels. I would recommend everyone interested in getting Lumina to undergo genetic testing beforehand.